Fepblue Prior Authorization Form
Fepblue Prior Authorization Form - Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web february 2019 addition of statement: Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. However, some select drugs require your doctor to provide information about your prescription to determine coverage. Effective on january 1, 2022 updated: Service benefit plan prior approval p.o. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Web get the latest from fep. Web fep prior approval program according to the terms of your coverage, prior approval is required for certain services and supplies and must be renewed periodically.
Web fep® blue focus www.fepblue.org 2023. Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Web fep prior approval program according to the terms of your coverage, prior approval is required for certain services and supplies and must be renewed periodically. December 23, 2021 prior approval is required for all imrt services except imrt related to the treatment of the. Brain cancer is not considered a form of head or neck cancer;. Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Web to request prior authorization for these medications, please submit the: Web most drugs are covered without requiring prior approval. However, some select drugs require your doctor to provide information about your prescription to determine coverage. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep).
Brain cancer is not considered a form of head or neck cancer;. Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Web fep® blue focus www.fepblue.org 2023. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Service benefit plan prior approval p.o. Web to request prior authorization for these medications, please submit the: Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web get the latest from fep.
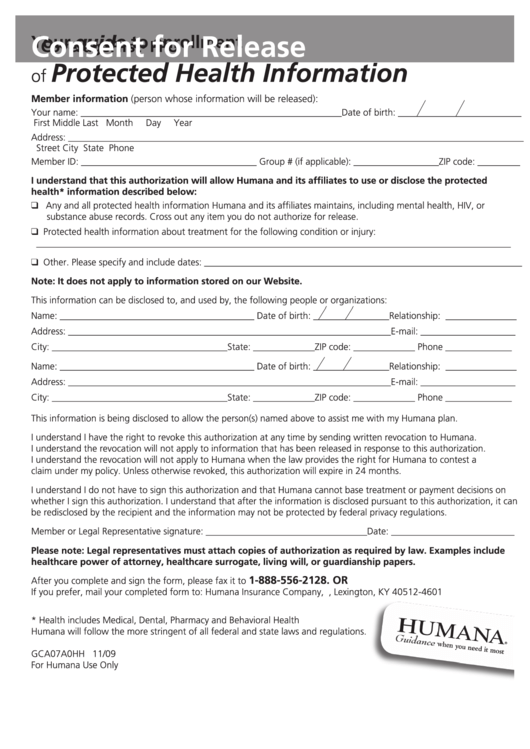
Fillable Consent For Release Of Protected Health Information printable
Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Service benefit plan prior approval p.o. Coronavirus update fep will waive early. Brain cancer is not considered a form of head or neck cancer;. Explore prior approval topics learn about prior.
Fep Prior Authorization Form â
Effective on january 1, 2022 updated: Web get the latest from fep. Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Brain cancer is not considered a form of head or neck cancer;. However, some select drugs require your doctor to provide information about your prescription to.
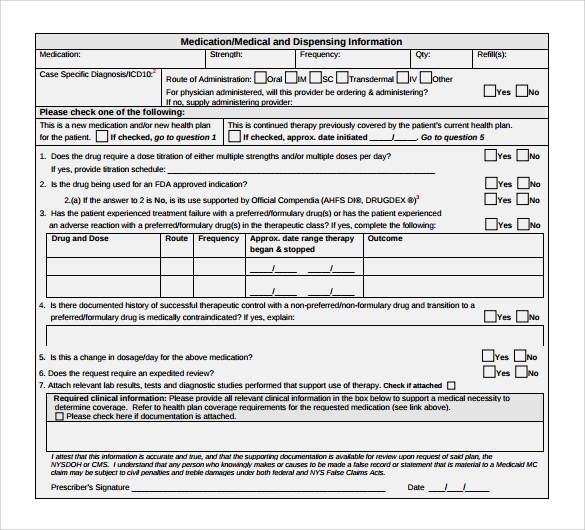
Medicare Generation Rx Prior Authorization Form Form Resume
December 23, 2021 prior approval is required for all imrt services except imrt related to the treatment of the. Web most drugs are covered without requiring prior approval. However, some select drugs require your doctor to provide information about your prescription to determine coverage. Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a.
Medicare Generation Rx Prior Authorization Form Form Resume
Service benefit plan prior approval p.o. Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure, service, or supply is provided. Brain cancer is not considered a form of head or neck cancer;. Web 2022 fep blue focus; Web pharmacy the blue cross and blue shield service benefit plan has a variety.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
However, some select drugs require your doctor to provide information about your prescription to determine coverage. Explore prior approval topics learn about prior. Service benefit plan prior approval p.o. Web standard and basic option prior approval list fep blue focus prior approval list. Web to request prior authorization for these medications, please submit the:
Covermymeds Prior Authorization Form Pdf Form Resume Examples
Web get the latest from fep. Service benefit plan prior approval p.o. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Web most drugs are covered without requiring prior approval. Web prior approval may be required for certain prescription drugs before they can be covered.
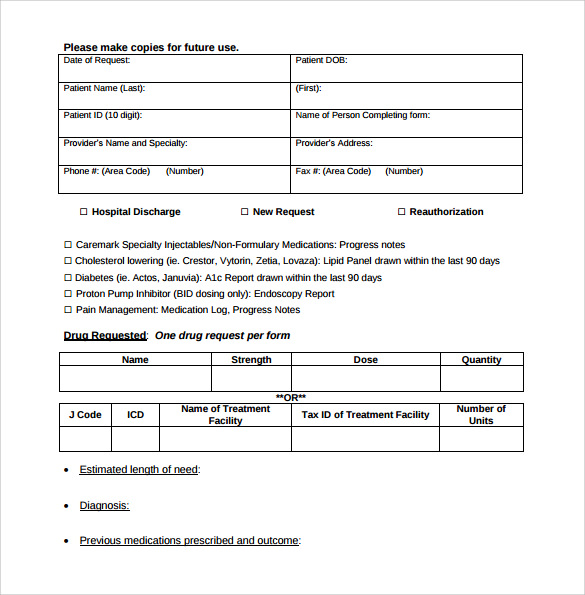
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Web the preferred provider network for fep is preferred patient care. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Coronavirus update fep will waive early. Brain cancer is not considered a form of head or neck cancer;.
Fep Blue Fill Online, Printable, Fillable, Blank pdfFiller
Web standard and basic option prior approval list fep blue focus prior approval list. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Coronavirus update fep will waive.
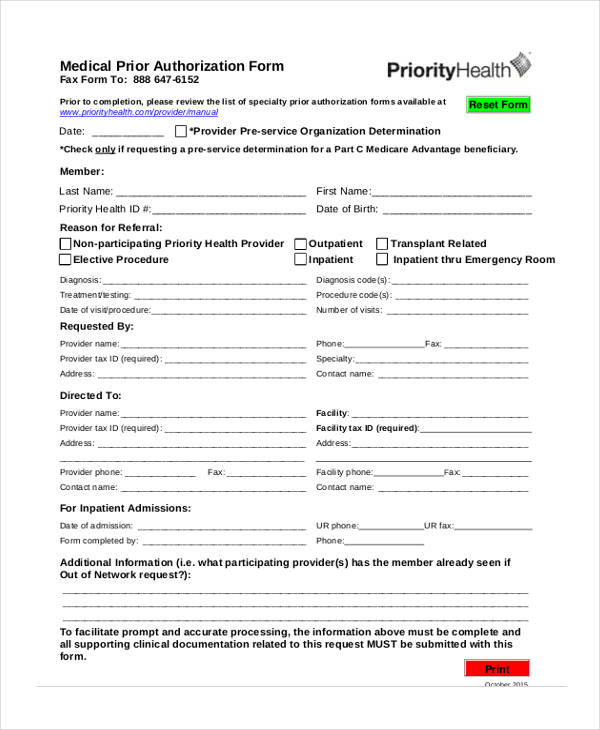
FREE 13+ Prior Authorization Forms in PDF MS Word
Web most drugs are covered without requiring prior approval. Web the preferred provider network for fep is preferred patient care. Web to request prior authorization for these medications, please submit the: Service benefit plan prior approval p.o. Explore prior approval topics learn about prior.
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Service benefit plan prior approval p.o. Web 1 results found for search term : Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Service benefit plan prior approval p.o.
Be The First To Know About Our Benefits, Wellness Incentives And Rewards You're Eligible For With Your Plan.
Service benefit plan prior approval p.o. Web 2022 fep blue focus; Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Web the preferred provider network for fep is preferred patient care.
Brain Cancer Is Not Considered A Form Of Head Or Neck Cancer;.
Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. However, some select drugs require your doctor to provide information about your prescription to determine coverage.
Explore Prior Approval Topics Learn About Prior.
Web to request prior authorization for these medications, please submit the: Web most drugs are covered without requiring prior approval. Service benefit plan prior approval p.o. Effective on january 1, 2022 updated:
Service Benefit Plan Prior Approval P.o.
Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure, service, or supply is provided. Web fep® blue focus www.fepblue.org 2023. Web fep prior approval program according to the terms of your coverage, prior approval is required for certain services and supplies and must be renewed periodically. Fep offers three nationwide options for federal employees and retirees (standard option, basic option.