Caresource Prior Authorization Form
Caresource Prior Authorization Form - Listed below are all the forms you may need as a caresource member. Web attach clinical notes with history and prior treatment. Illegible or incomplete forms will be returned. Web the best way to modify and esign caresource imaging prior authorization form without breaking a sweat. Web we want you to easily find the forms you need for your caresource plan. Make use of the tools we offer to fill out your form. Prior authorization requests without medical justification or previous medications listed will be considered incomplete; Save or instantly send your ready documents. Services billed must be within the provider’s scope of practice as determined by the applicable fee/payment schedule and the claim timely filing limits. Locate rad md prior auth imaging caresource and click on get form to get started.
Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web caresource prior authorization prior authorization (pa) is how we decide if the health services listed below will be covered by your caresource plan. Easily fill out pdf blank, edit, and sign them. To see the full list of forms for your plan, please select your plan from the drop down list above. Web we want you to easily find the forms you need for your caresource plan. Locate rad md prior auth imaging caresource and click on get form to get started. Your provider must get prior authorization before you get any of these services. Web the best way to modify and esign caresource imaging prior authorization form without breaking a sweat. Web approved prior authorization payment is contingent upon the eligibility of the member at the time of service. Save or instantly send your ready documents.
Locate rad md prior auth imaging caresource and click on get form to get started. Make use of the tools we offer to fill out your form. Web approved prior authorization payment is contingent upon the eligibility of the member at the time of service. Save or instantly send your ready documents. Illegible or incomplete forms will be returned. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. They must also fall within the terms Web select the appropriate caresource form to get started. Covermymeds is caresource prior authorization forms’s preferred method for receiving epa requests. Web caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits.
Bcbs Prior Authorization Form Michigan Form Resume Examples kDp3Og030Q
Web we want you to easily find the forms you need for your caresource plan. Illegible or incomplete forms will be returned. Web attach clinical notes with history and prior treatment. To see the full list of forms for your plan, please select your plan from the drop down list above. Covermymeds is caresource prior authorization forms’s preferred method for.
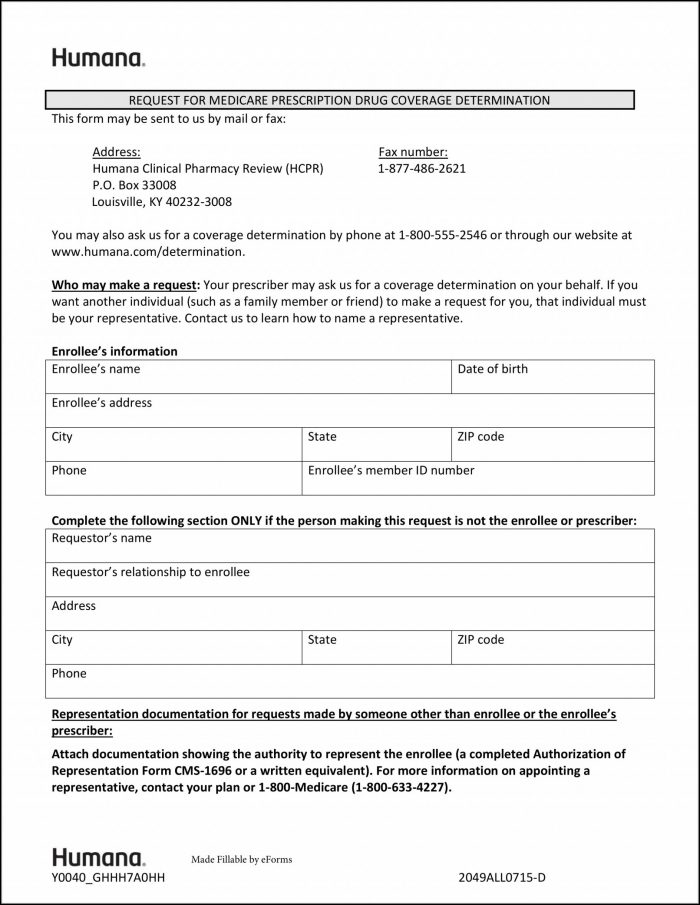
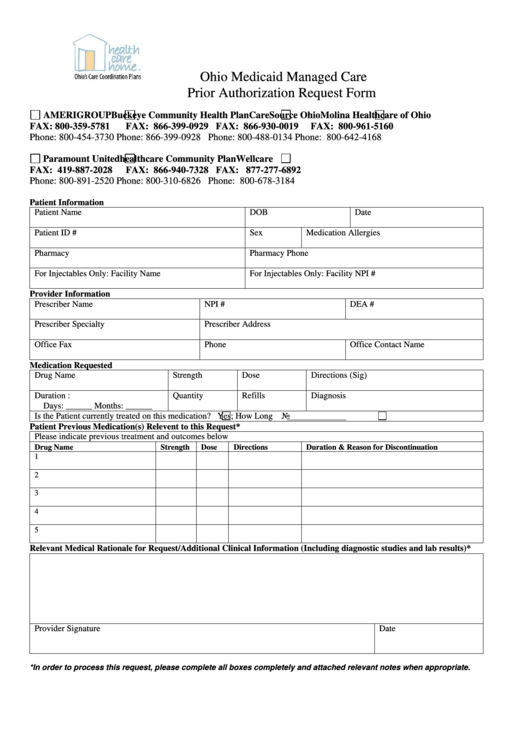
Prior Authorization Request Form printable pdf download
They must also fall within the terms Web we want you to easily find the forms you need for your caresource plan. Illegible or incomplete forms will be returned. Services billed must be within the provider’s scope of practice as determined by the applicable fee/payment schedule and the claim timely filing limits. Web caresource prior authorization prior authorization (pa) is.
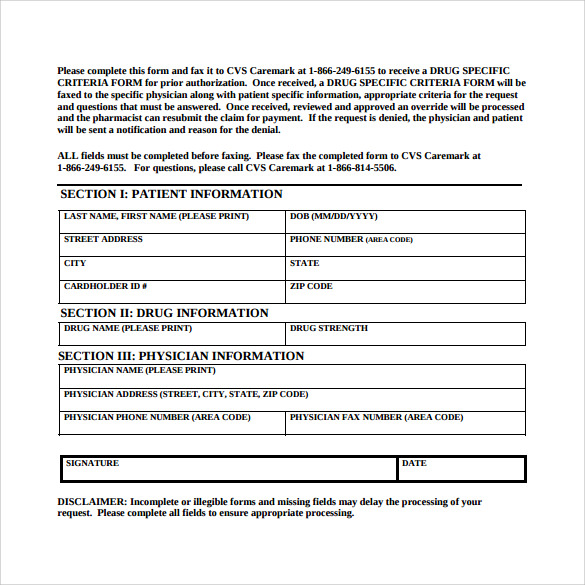
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF
Listed below are all the forms you may need as a caresource member. Save or instantly send your ready documents. Web caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Covermymeds is caresource prior authorization forms’s preferred method for receiving epa requests. Prior authorization requests without medical justification or previous medications listed will be considered.
Work From Home Prior Authorization Jobs — Intake Agent Prior
Locate rad md prior auth imaging caresource and click on get form to get started. Web select the appropriate caresource form to get started. They must also fall within the terms Services billed must be within the provider’s scope of practice as determined by the applicable fee/payment schedule and the claim timely filing limits. Web caresource® evaluates prior authorization requests.
Fillable Online Ohio Provider Medical Prior Authorization Request Form
Listed below are all the forms you may need as a caresource member. Covermymeds is caresource prior authorization forms’s preferred method for receiving epa requests. They must also fall within the terms To see the full list of forms for your plan, please select your plan from the drop down list above. Web caresource prior authorization prior authorization (pa) is.
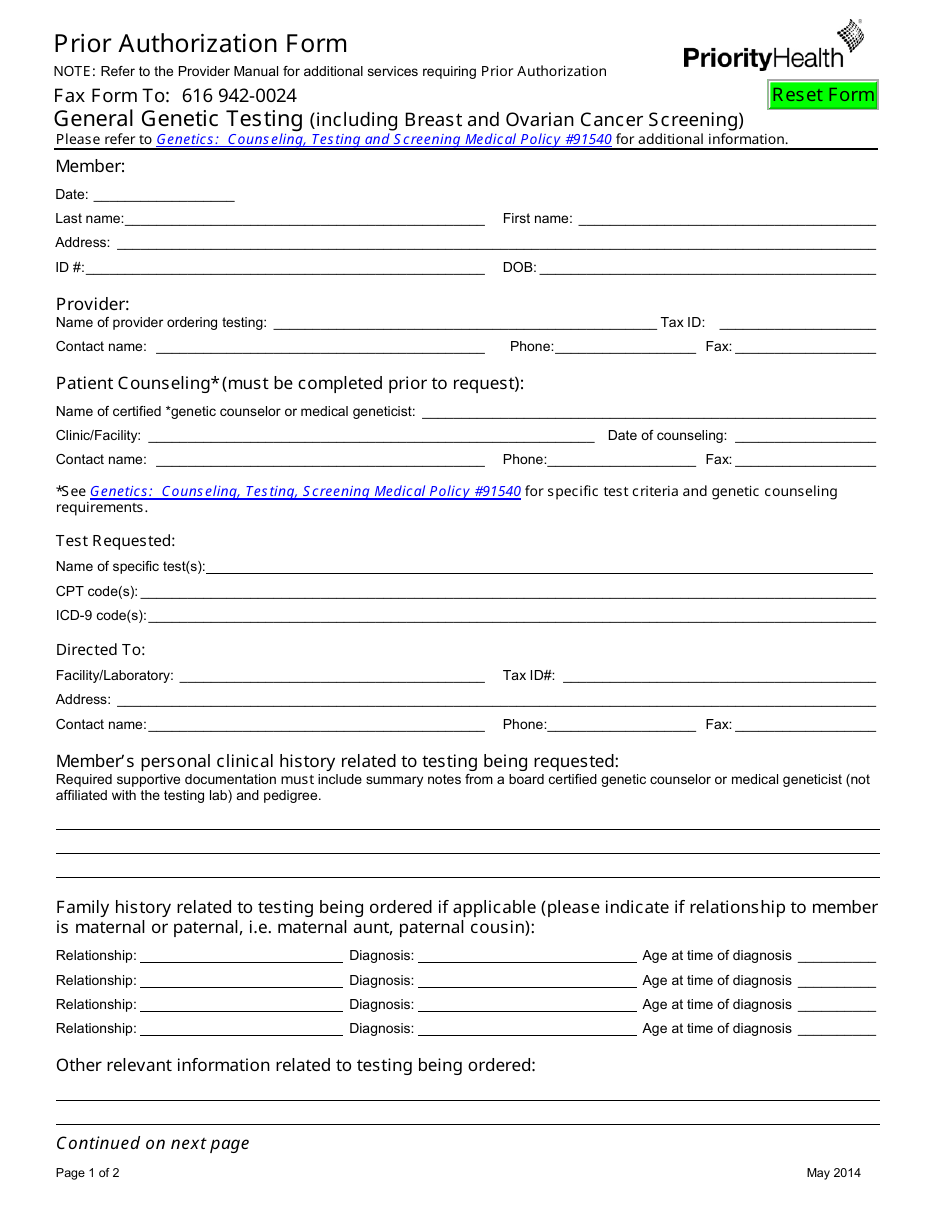
Prior Authorization Form Priorityhealth Download Fillable PDF
Web attach clinical notes with history and prior treatment. Covermymeds is caresource prior authorization forms’s preferred method for receiving epa requests. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. To see the.
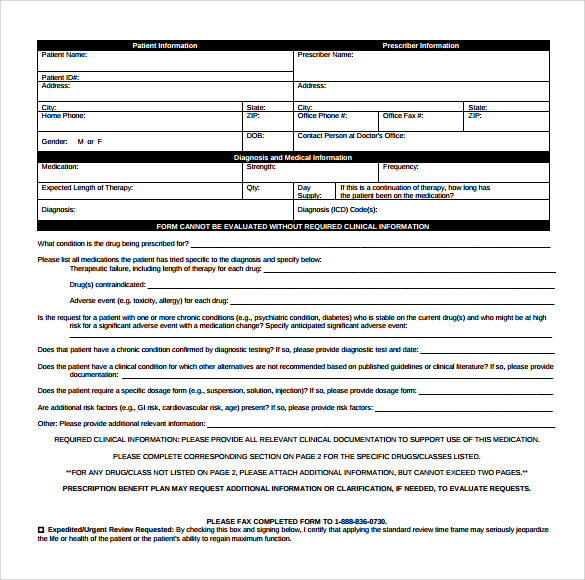
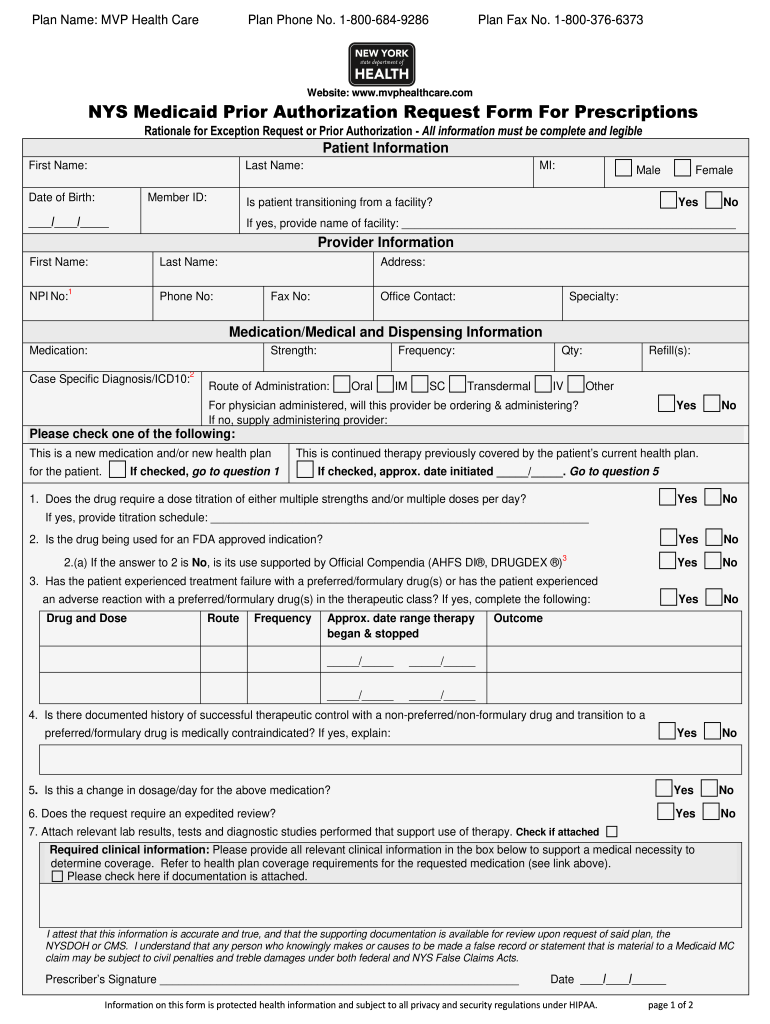
Pharmacy Prior Authorization Form Sample Templates
Make use of the tools we offer to fill out your form. They must also fall within the terms Prior authorization requests without medical justification or previous medications listed will be considered incomplete; Covermymeds is caresource prior authorization forms’s preferred method for receiving epa requests. Listed below are all the forms you may need as a caresource member.
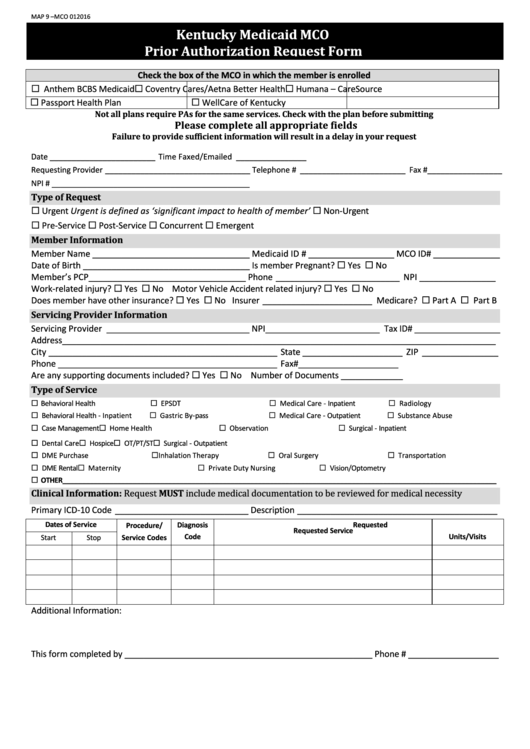
Fillable Kentucky Medicaid Mco Prior Authorization Request Form
Web caresource prior authorization prior authorization (pa) is how we decide if the health services listed below will be covered by your caresource plan. Services billed must be within the provider’s scope of practice as determined by the applicable fee/payment schedule and the claim timely filing limits. Covermymeds is caresource prior authorization forms’s preferred method for receiving epa requests. Covermymeds.
Caremore Prior Authorization Form Fill Out and Sign Printable PDF
Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web we want you to easily find the forms you need for your caresource plan. Web caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Easily fill out pdf blank, edit, and sign them..
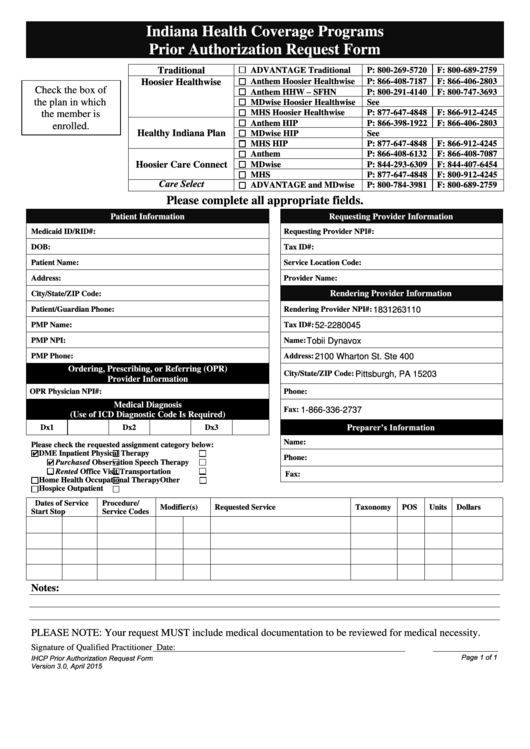
Fillable Indiana Health Coverage Programs Prior Authorization Request
Prior authorization requests without medical justification or previous medications listed will be considered incomplete; Services billed must be within the provider’s scope of practice as determined by the applicable fee/payment schedule and the claim timely filing limits. Make use of the tools we offer to fill out your form. Web attach clinical notes with history and prior treatment. Web we.
They Must Also Fall Within The Terms
Save or instantly send your ready documents. Web attach clinical notes with history and prior treatment. Web the best way to modify and esign caresource imaging prior authorization form without breaking a sweat. Web caresource prior authorization prior authorization (pa) is how we decide if the health services listed below will be covered by your caresource plan.
Web Select The Appropriate Caresource Form To Get Started.
To see the full list of forms for your plan, please select your plan from the drop down list above. Your provider must get prior authorization before you get any of these services. Locate rad md prior auth imaging caresource and click on get form to get started. Illegible or incomplete forms will be returned.
Easily Fill Out Pdf Blank, Edit, And Sign Them.
Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Make use of the tools we offer to fill out your form. Services billed must be within the provider’s scope of practice as determined by the applicable fee/payment schedule and the claim timely filing limits. Web approved prior authorization payment is contingent upon the eligibility of the member at the time of service.
Covermymeds Is Caresource Prior Authorization Forms’s Preferred Method For Receiving Epa Requests.
Listed below are all the forms you may need as a caresource member. Web caresource® evaluates prior authorization requests based on medical necessity, medical appropriateness and benefit limits. Prior authorization requests without medical justification or previous medications listed will be considered incomplete; Web we want you to easily find the forms you need for your caresource plan.