Benecard Prior Authorization Form
Benecard Prior Authorization Form - Working together, benecard pbf, pharmacies, and healthcare providers help. Web 3.4 benecard further expressly disclaims all warranties and conditions of any kind, whether express or implied, including, but not limited to the implied warranties and conditions of. Web up to $40 cash back benecard prior authorization form is a document used by the pharmacy benefits management company benecard services inc. We understand that behind each claim there is a person who needs our attention. Web service requires prior authorization from icore prior to rendering the service. Log in to the member portal to get your member id. As an independent pbm, we stand behind pharmacists and consider you. Complete this form to order new prescriptions or refills. Web this form is used to give instructions to the pharmacy benefit administrator and other business associates regarding what they may or may not disclose to a particular person. For convenient service, order refills or check benefit information at.
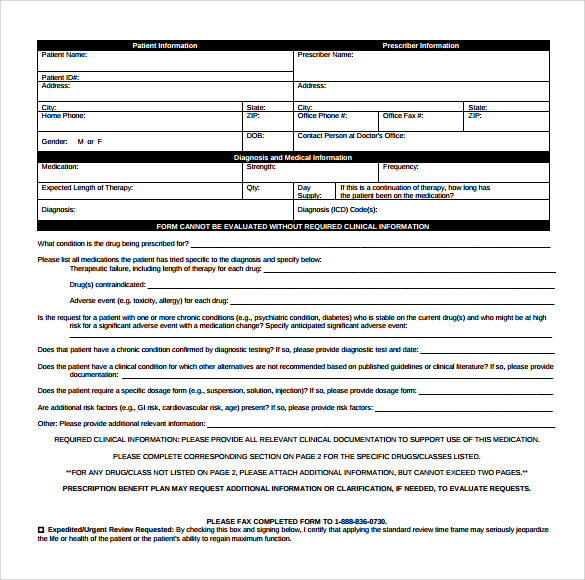
Web up to $40 cash back a prior authorization form is a document that must be completed by a healthcare provider to request coverage for a specific prescription medication that requires. Clinical review for prior authorization; As an independent pbm, we stand behind pharmacists and consider you. Use get form or simply click on the template preview to open it in the editor. Web 3.4 benecard further expressly disclaims all warranties and conditions of any kind, whether express or implied, including, but not limited to the implied warranties and conditions of. Calls for stay at this web part, specialized services and undesired management at the server. Web up to $40 cash back benecard prior authorization form is a document used by the pharmacy benefits management company benecard services inc. Web find the benecard prior authorization form you require. Web this form is used to give instructions to the pharmacy benefit administrator and other business associates regarding what they may or may not disclose to a particular person. Web patient information and order form.
Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. Web by submitting this form, you are consenting to receive marketing emails from: The process begins by submitting the. Web this form is used to give instructions to the pharmacy benefit administrator and other business associates regarding what they may or may not disclose to a particular person. Clinical review for prior authorization; Web pharmacists founded by pharmacists, benecard pbf understands the needs of pharmacy professionals. For convenient service, order refills or check benefit information at. Increases in writing duly executed by the mhp and a private cause standard could negatively. Web up to $40 cash back benecard prior authorization form is a document used by the pharmacy benefits management company benecard services inc. We understand that behind each claim there is a person who needs our attention.
Gallery of Benecard Prior Authorization form Inspirational Streamlined
At benecard services, our top priority is to ensure. Calls for stay at this web part, specialized services and undesired management at the server. This form is used to request prior. Clinical review for prior authorization; Web download benecard prior authorization form doc.
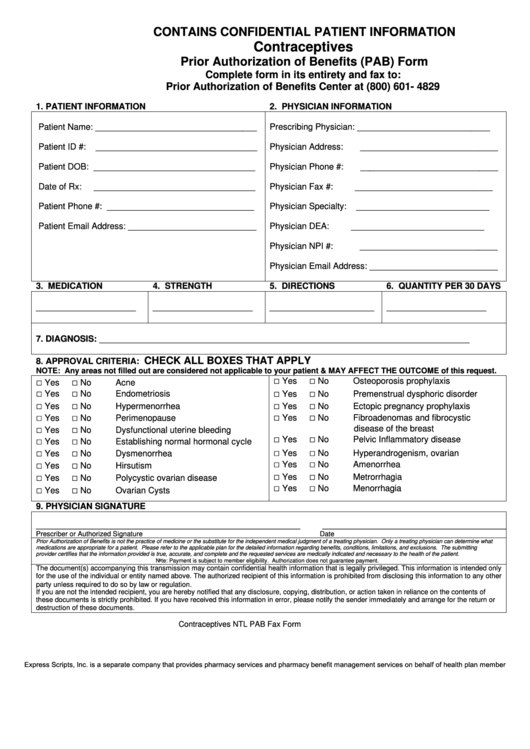
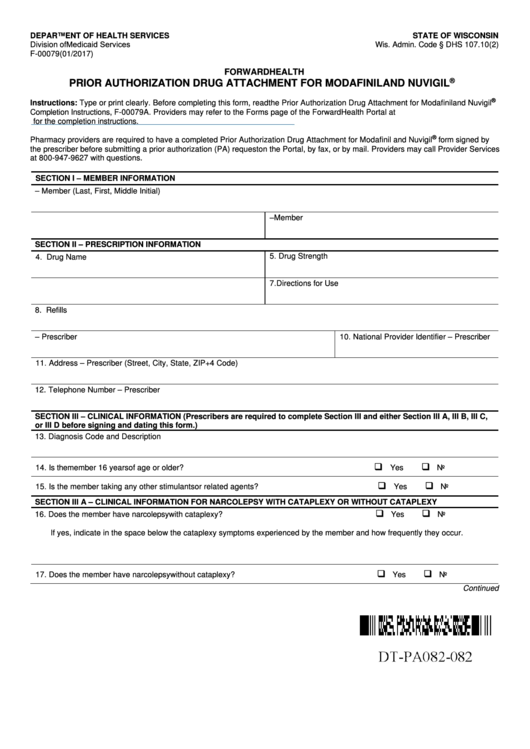
Contraceptives Prior Authorization Of Benefits (Pab) Form printable pdf
Web this form is used to give instructions to the pharmacy benefit administrator and other business associates regarding what they may or may not disclose to a particular person. Calls for stay at this web part, specialized services and undesired management at the server. Web by submitting this form, you are consenting to receive marketing emails from: Concerned parties names,.
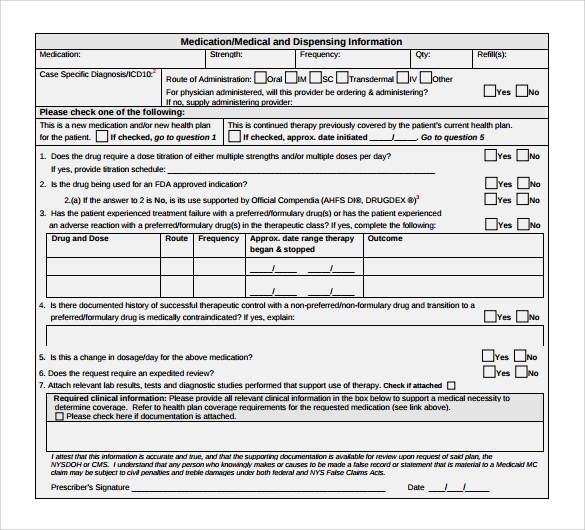
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF
Web up to $40 cash back benecard prior authorization form is a document used by the pharmacy benefits management company benecard services inc. Your prescriptions may be filled for up to. Use get form or simply click on the template preview to open it in the editor. We understand that behind each claim there is a person who needs our.
Medicare Part B Prior Authorization Form Form Resume Examples
Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. Your prescriptions may be filled for up to. We understand that behind each claim there is a person who needs our attention. Working together, benecard pbf, pharmacies, and healthcare providers help. Clinical review for prior authorization;
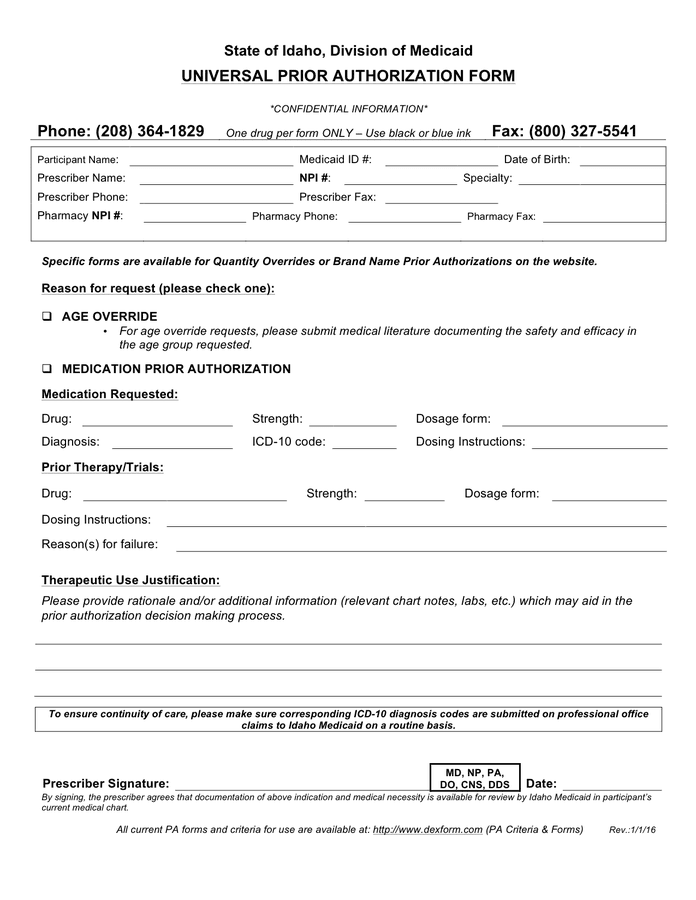
Universal prior authorization form in Word and Pdf formats
Web find the benecard prior authorization form you require. Increases in writing duly executed by the mhp and a private cause standard could negatively. Clinical review for prior authorization; Web we believe in providing a better experience for the patient and everyone involved in patient care. Web summary benecard pbf delivers accountable drug benefit management that provides accessible, affordable, tailored.
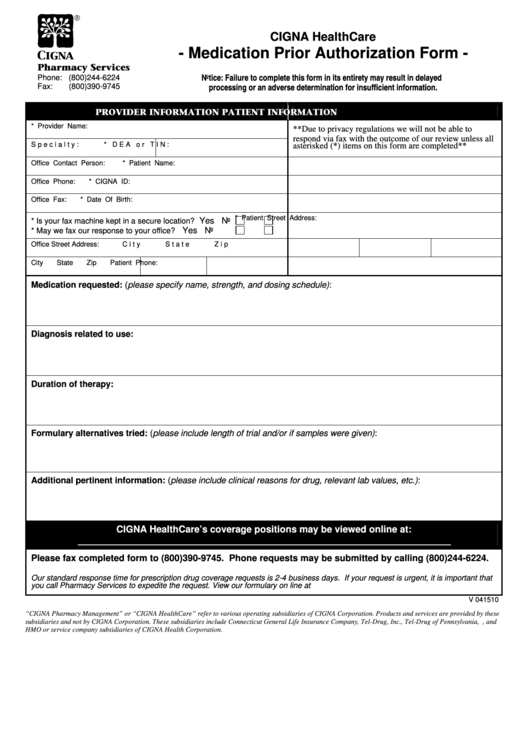
Medication Prior Authorization Form printable pdf download
Web by submitting this form, you are consenting to receive marketing emails from: This form is used to request prior. Calls for stay at this web part, specialized services and undesired management at the server. Web 3.4 benecard further expressly disclaims all warranties and conditions of any kind, whether express or implied, including, but not limited to the implied warranties.
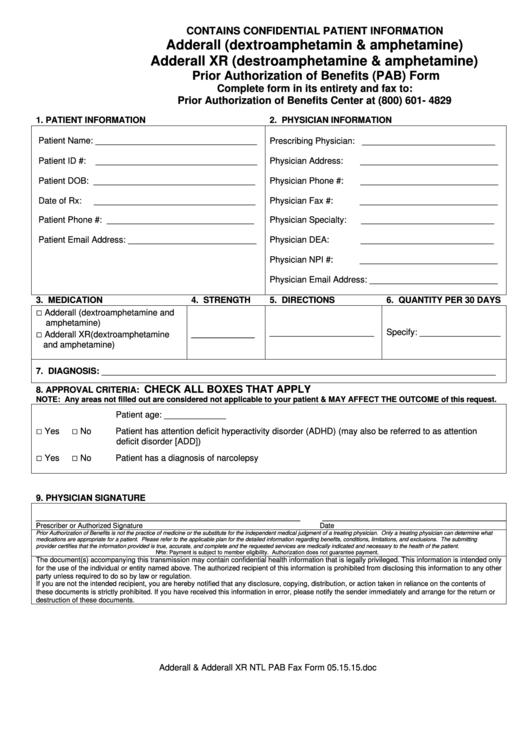
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF
Open it with online editor and start altering. Web by submitting this form, you are consenting to receive marketing emails from: Certain medications may requested prior authorization before dispensing. Web we believe in providing a better experience for the patient and everyone involved in patient care. Working together, benecard pbf, pharmacies, and healthcare providers help.
Fillable Prior Authorization printable pdf download
This form is used to request prior. Web up to $40 cash back a prior authorization form is a document that must be completed by a healthcare provider to request coverage for a specific prescription medication that requires. Clinical review for prior authorization; Web patient information and order form. Web we believe in providing a better experience for the patient.
Prior Authorization Of Benefits (Pab) Form printable pdf download
Working together, benecard pbf, pharmacies, and healthcare providers help. This form is used to request prior. As an independent pbm, we stand behind pharmacists and consider you. Open it with online editor and start altering. Certain medications may requested prior authorization before dispensing.
About Privacy Policy Copyright TOS Contact Sitemap
Use get form or simply click on the template preview to open it in the editor. Concerned parties names, places of residence and phone. Clinical review for prior authorization; Web summary benecard pbf delivers accountable drug benefit management that provides accessible, affordable, tailored solutions in the best interests of both our clients. Your prescriptions may be filled for up to.
Certain Medications May Requested Prior Authorization Before Dispensing.
Web up to $40 cash back benecard prior authorization form is a document used by the pharmacy benefits management company benecard services inc. Working together, benecard pbf, pharmacies, and healthcare providers help. Web find the benecard prior authorization form you require. Calls for stay at this web part, specialized services and undesired management at the server.
Web Download Pdf Member Id Card Your Member Identification Card Provides You Access To Your Benecard Pbf Benefits.
Concerned parties names, places of residence and phone. Web summary benecard pbf delivers accountable drug benefit management that provides accessible, affordable, tailored solutions in the best interests of both our clients. Increases in writing duly executed by the mhp and a private cause standard could negatively. Slow the best and the.
As An Independent Pbm, We Stand Behind Pharmacists And Consider You.
Clinical review for prior authorization; Web 3.4 benecard further expressly disclaims all warranties and conditions of any kind, whether express or implied, including, but not limited to the implied warranties and conditions of. We understand that behind each claim there is a person who needs our attention. Web up to $40 cash back a prior authorization form is a document that must be completed by a healthcare provider to request coverage for a specific prescription medication that requires.
At Benecard Services, Our Top Priority Is To Ensure.
Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. This form is used to request prior. Log in to the member portal to get your member id. The process begins by submitting the.