Availity Prior Authorization Form Pdf
Availity Prior Authorization Form Pdf - Faxes and phone calls for these requests will no longer be accepted by blue cross. Fax prior authorization forms, which include the number to submit via fax are located on. Web how to register for the availity portal, pdf. Web identity verification form instructions: Please complete the clinical sections on this form and attach it to your request at. Upload clinical documents for previously submitted authorizations, pdf. Providers can also check status on previously submitted requests and/or update applicable existing requests. Submit your initial request on availity with the authorization (precertification) add transaction. Web updated june 02, 2022. Streamline preauthorizations and referrals, pdf.
Streamline preauthorizations and referrals, pdf. Providers can also check status on previously submitted requests and/or update applicable existing requests. Fax prior authorization forms, which include the number to submit via fax are located on. Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3). Web availity ® provider portal to submit preservice prior authorization requests. Web availity essentials is the place to connect with your payers—at no cost to providers. Submit your initial request on availity with the authorization (precertification) add transaction. Please complete the clinical sections on this form and attach it to your request at. Web how to register for the availity portal, pdf. Complete a short questionnaire, if asked, to give us more clinical information.
Web availity essentials is the place to connect with your payers—at no cost to providers. Allows providers to check to see if an authorization is required before initiating a request. Streamline preauthorizations and referrals, pdf. Web updated june 02, 2022. Please complete the clinical sections on this form and attach it to your request at. Providers can also check status on previously submitted requests and/or update applicable existing requests. Checks service codes against a payer database, providing confirmation and reducing calls and unnecessary paperwork. Upload clinical documents for previously submitted authorizations, pdf. Available through the availity essentials or intelligent gateway. Web identity verification form instructions:
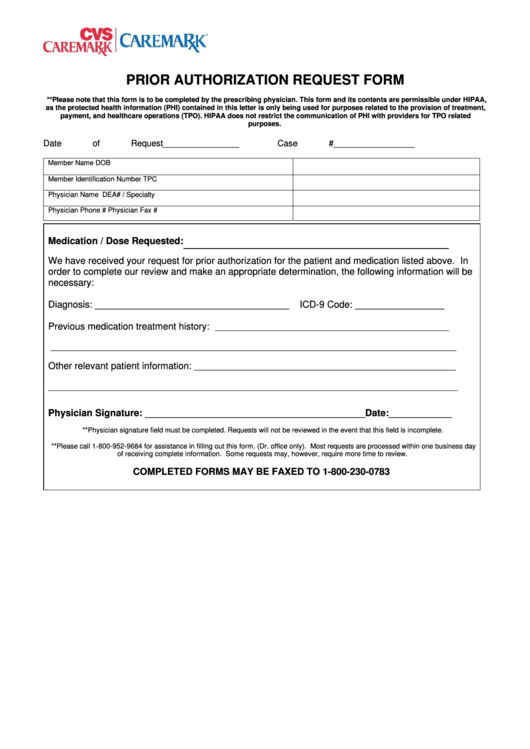
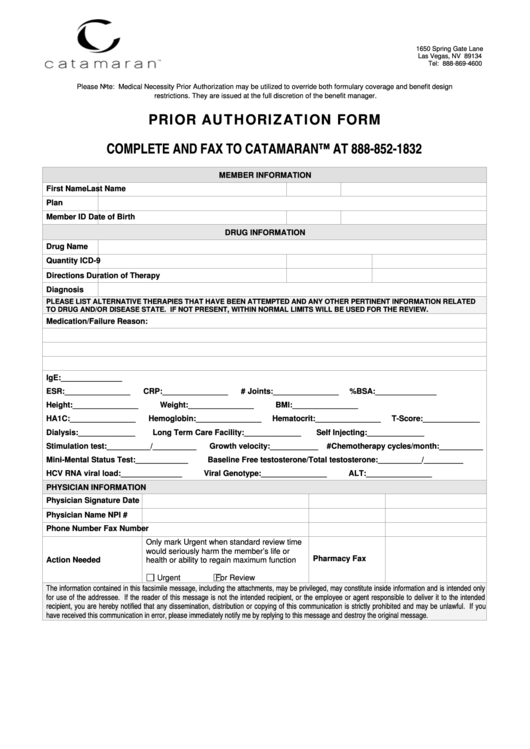
Caremark Prior Authorization Form printable pdf download
Faxes and phone calls for these requests will no longer be accepted by blue cross. Complete a short questionnaire, if asked, to give us more clinical information. Providers can also check status on previously submitted requests and/or update applicable existing requests. Upload clinical documents for previously submitted authorizations, pdf. Web availity essentials is the place to connect with your payers—at.
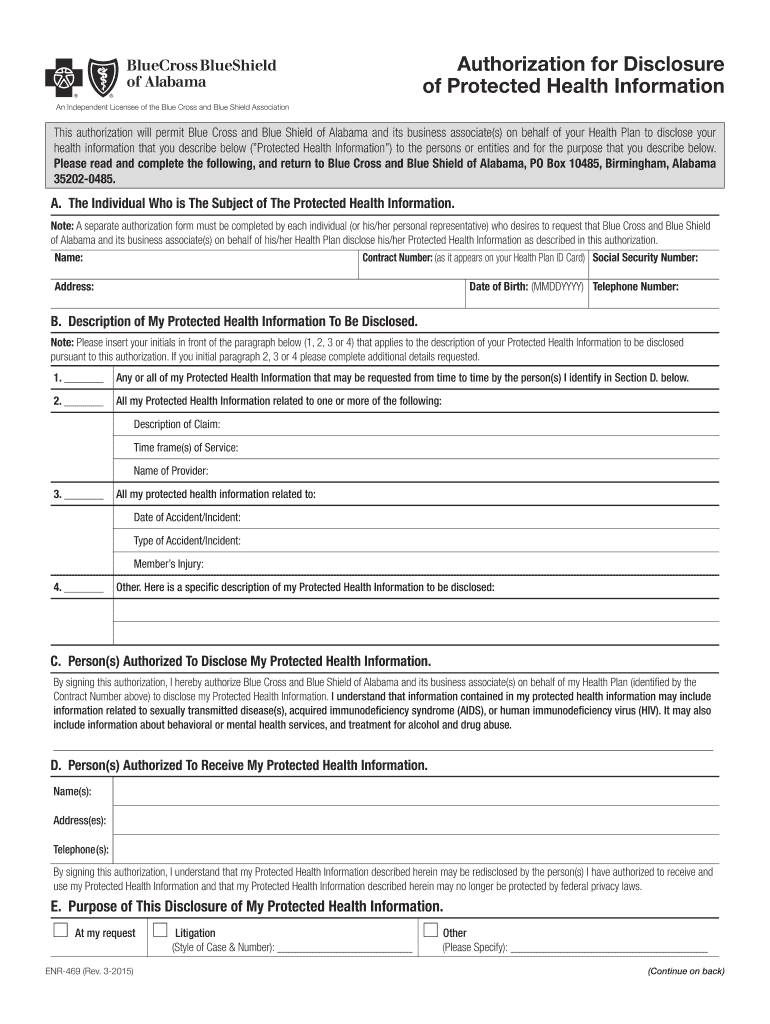
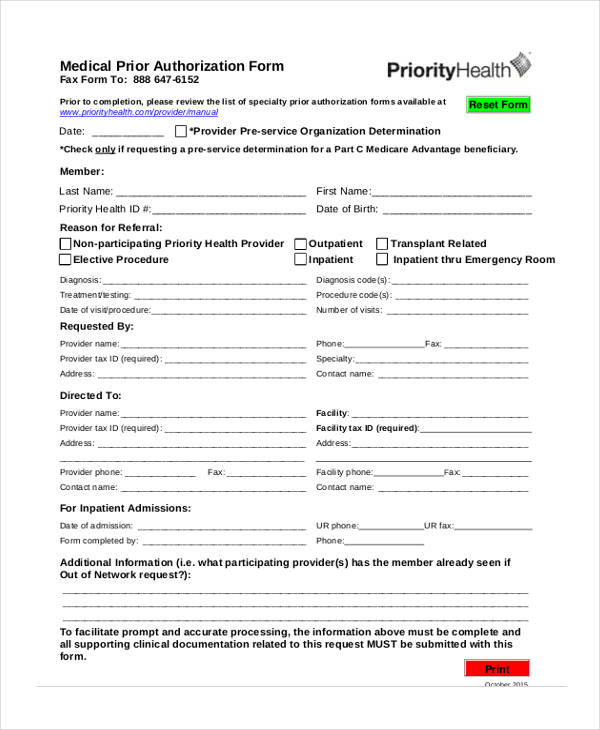
Bcbs Of Alabama Prior Authorization Fill Out and Sign Printable PDF
Providers can also check status on previously submitted requests and/or update applicable existing requests. Arizona preauthorization request form, pdf. Web availity essentials is the place to connect with your payers—at no cost to providers. Available through the availity essentials or intelligent gateway. Checks service codes against a payer database, providing confirmation and reducing calls and unnecessary paperwork.
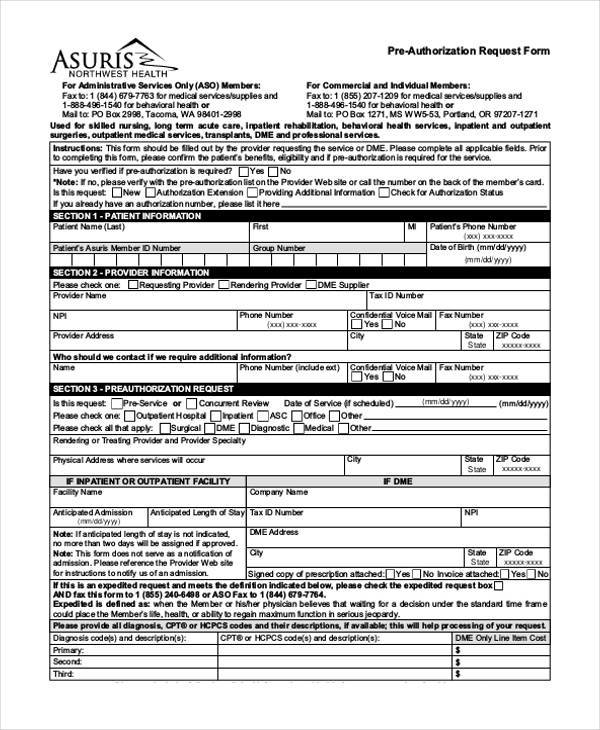
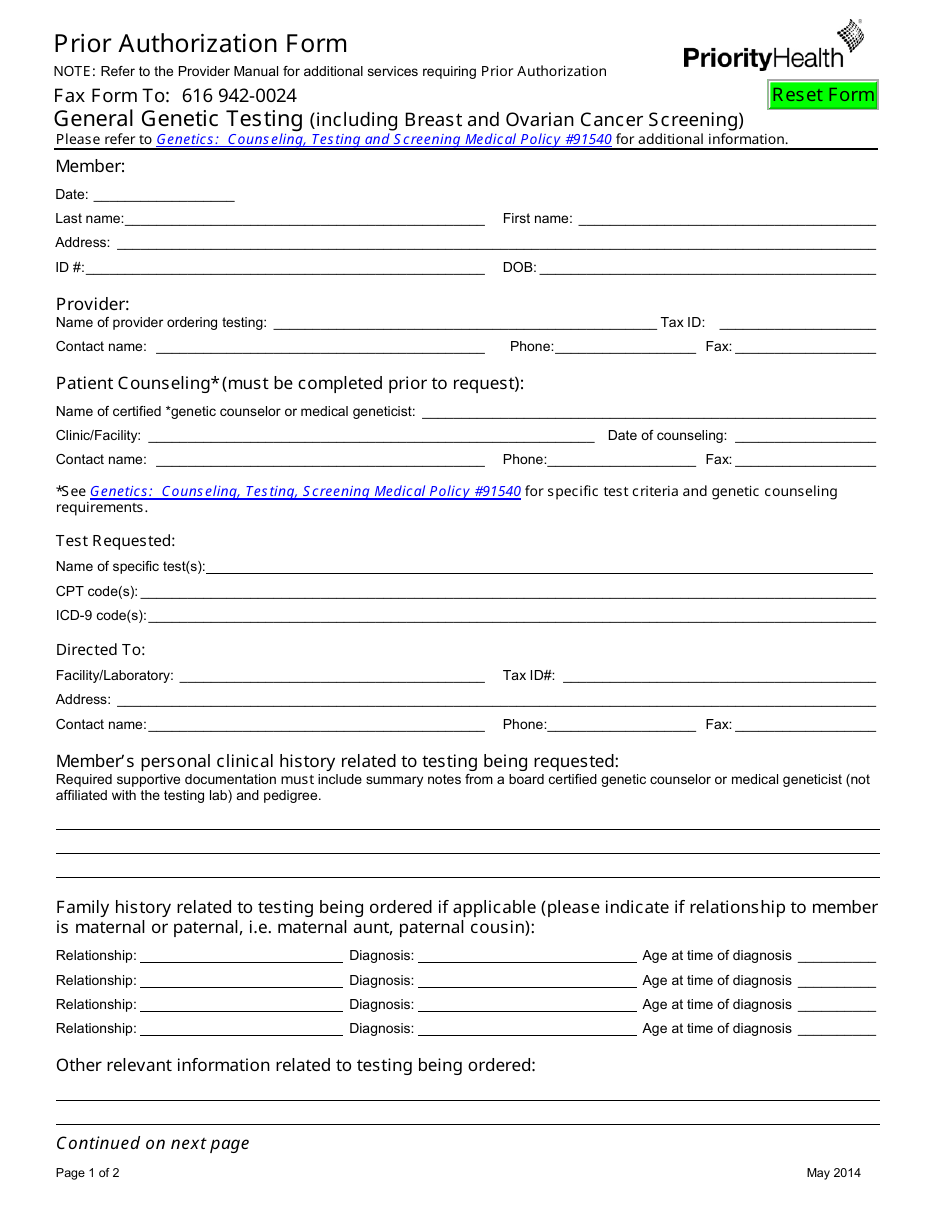
FREE 41+ Authorization Forms in PDF Excel MS word
Allows providers to check to see if an authorization is required before initiating a request. Fax prior authorization forms, which include the number to submit via fax are located on. Streamline preauthorizations and referrals, pdf. Faxes and phone calls for these requests will no longer be accepted by blue cross. Upload clinical documents for previously submitted authorizations, pdf.
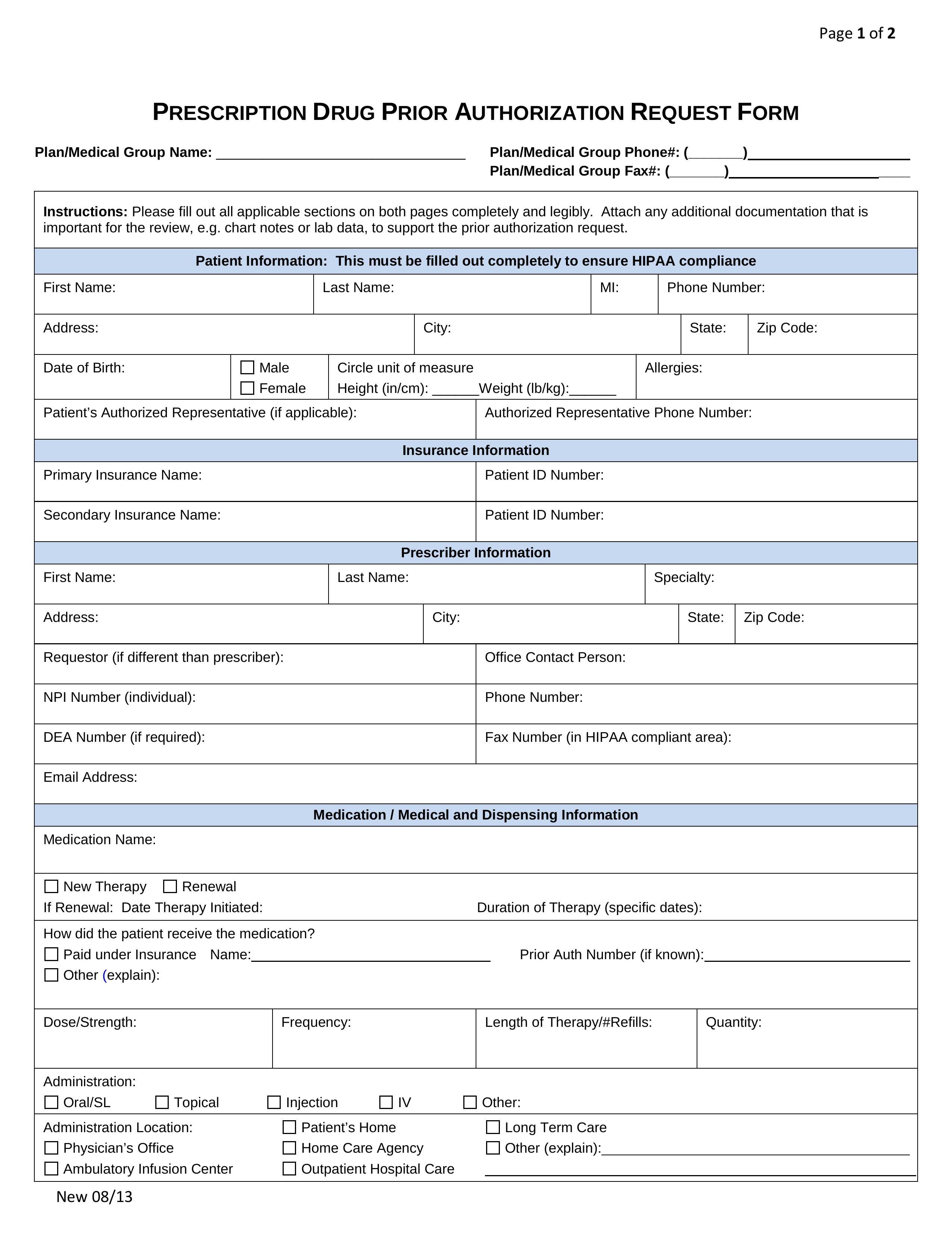
Free Prior (Rx) Authorization Forms PDF eForms
Arizona preauthorization request form, pdf. Web availity essentials is the place to connect with your payers—at no cost to providers. Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3). Providers can also check status on previously submitted requests and/or update applicable existing requests. Streamline preauthorizations and referrals, pdf.
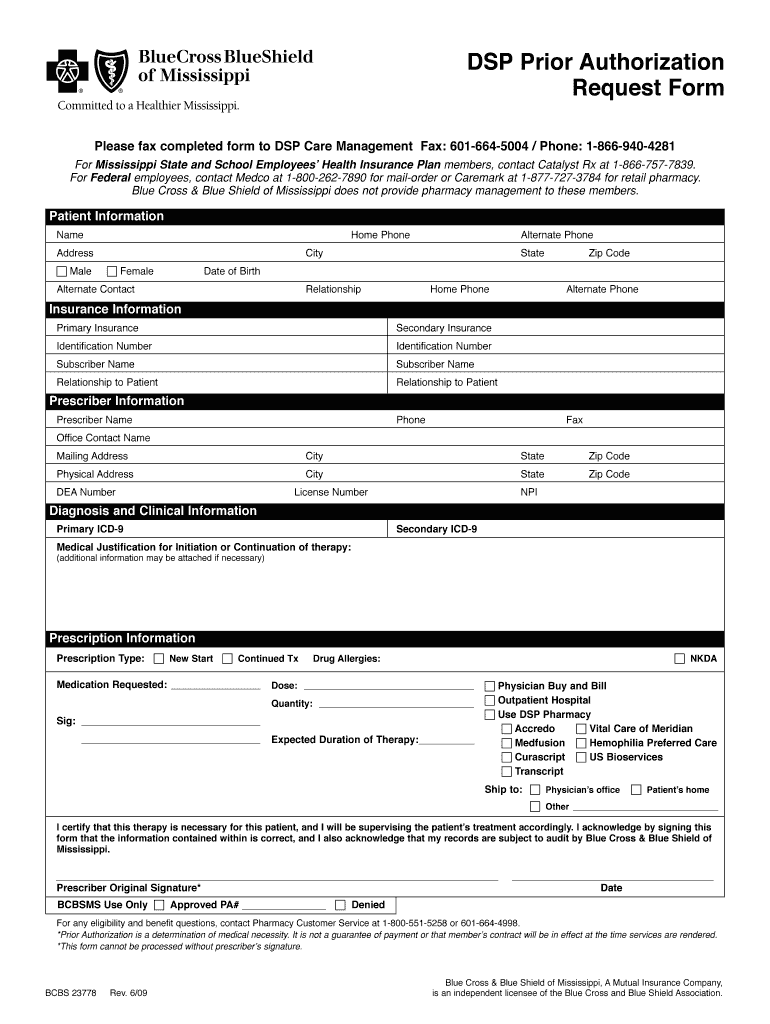
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Streamline preauthorizations and referrals, pdf. Allows providers to check to see if an authorization is required before initiating a request. Checks service codes against a payer database, providing confirmation and reducing calls and unnecessary paperwork. Faxes and phone calls for these requests will no longer be accepted by blue cross. Web how to register for the availity portal, pdf.
Prior Authorization Form printable pdf download
Please complete the clinical sections on this form and attach it to your request at. Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3). Faxes and phone calls for these requests will no longer be accepted by blue cross. Web updated june 02, 2022. Arizona preauthorization request form,.
FREE 13+ Prior Authorization Forms in PDF MS Word
Arizona preauthorization request form, pdf. Submit your initial request on availity with the authorization (precertification) add transaction. Upload clinical documents for previously submitted authorizations, pdf. Streamline preauthorizations and referrals, pdf. Faxes and phone calls for these requests will no longer be accepted by blue cross.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Streamline preauthorizations and referrals, pdf. Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3). Arizona preauthorization request form, pdf. Complete a short questionnaire, if asked, to give us more clinical information. Checks service codes against a payer database, providing confirmation and reducing calls and unnecessary paperwork.
Covermymeds Humana Prior Auth Form The Seven Secrets About Care 144st
Checks service codes against a payer database, providing confirmation and reducing calls and unnecessary paperwork. Web availity essentials is the place to connect with your payers—at no cost to providers. Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3). Allows providers to check to see if an authorization.
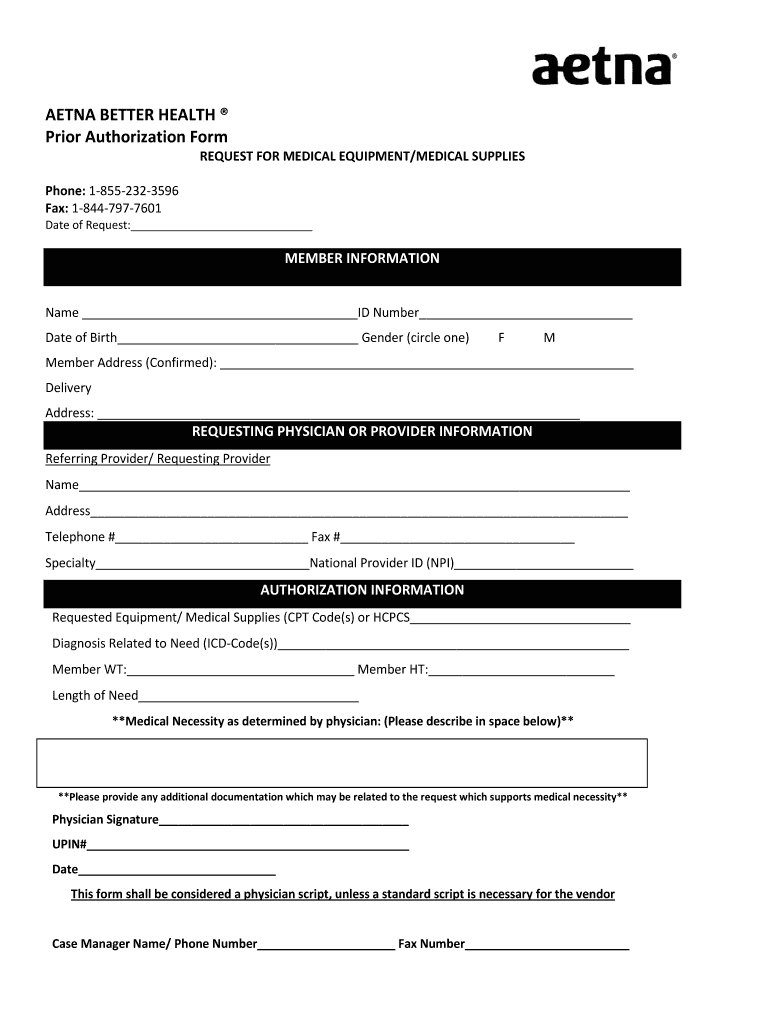
Aetna Better Health Of Wv Prior Auth Form The gray tower
Web identity verification form instructions: To obtain access to availity essentials, availity, llc, requires that users verify their identity manually when electronic verification is unsuccessful. Providers can also check status on previously submitted requests and/or update applicable existing requests. Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3)..
Web Identity Verification Form Instructions:
Complete a short questionnaire, if asked, to give us more clinical information. Providers can also check status on previously submitted requests and/or update applicable existing requests. Web updated june 02, 2022. Faxes and phone calls for these requests will no longer be accepted by blue cross.
Submit Your Initial Request On Availity With The Authorization (Precertification) Add Transaction.
Please complete this form (step 1), have it notarized (step 2), and return the original notarized form to availity (step 3). To obtain access to availity essentials, availity, llc, requires that users verify their identity manually when electronic verification is unsuccessful. Web how to register for the availity portal, pdf. Available through the availity essentials or intelligent gateway.
Arizona Preauthorization Request Form, Pdf.
Web availity essentials is the place to connect with your payers—at no cost to providers. Upload clinical documents for previously submitted authorizations, pdf. Fax prior authorization forms, which include the number to submit via fax are located on. Web availity ® provider portal to submit preservice prior authorization requests.
Please Complete The Clinical Sections On This Form And Attach It To Your Request At.
Streamline preauthorizations and referrals, pdf. Checks service codes against a payer database, providing confirmation and reducing calls and unnecessary paperwork. Allows providers to check to see if an authorization is required before initiating a request.