Ascension Complete Prior Authorization Form
Ascension Complete Prior Authorization Form - Web clinicians can submit requests: We require you to get. Web ascension complete will continue to perform prior authorization of coverage for interventional imaging procedures (even those that utilize mr/ct technology) prior. Web object moved to here. Web however, a completed written authorization is required prior to processing a request. Web what is the process for obtaining a prior authorization? You may opt out of future communications at any time. Web our plan has a team of doctors and pharmacists who create tools to help us provide you quality coverage. The um provider portal is an all access entry into your prior authorization requests and determinations. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage.
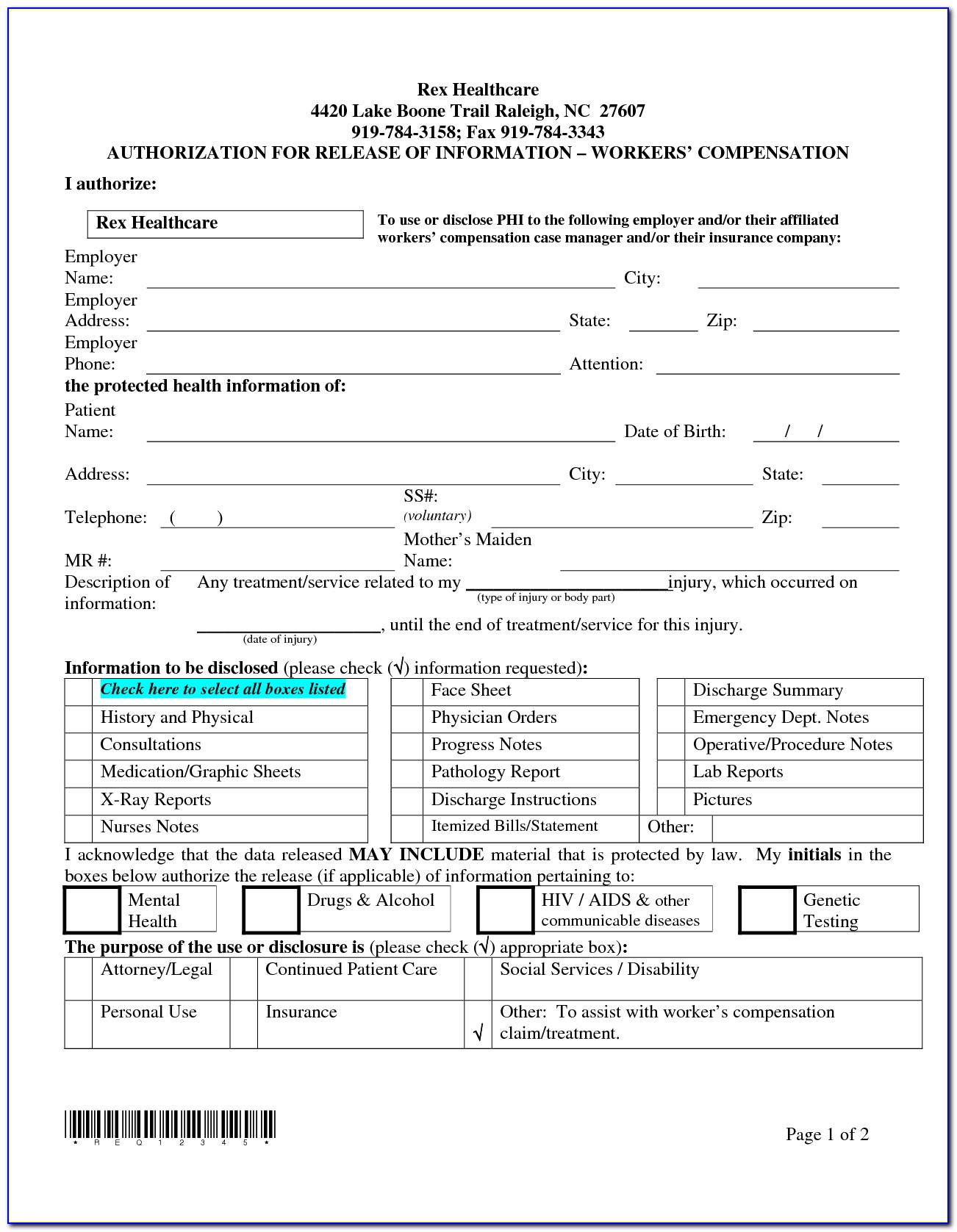
Web this documentation includes the following: Web provider resources | ascension complete | 2020 prior authorization forms medicare parts: Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. • smarthealth prior authorization form filled out in its entirety • clinical notes outlining symptoms and their duration • physical exam. • diagnostic imaging (mr, ct/cta, ccta, pet, myocardial. Protect yourself against medicare fraud and identifies. By portal view the status of an authorization by visiting the clinician portal by fax fax a completed prior authorization form to: Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web object moved to here. We require you to get.
• diagnostic imaging (mr, ct/cta, ccta, pet, myocardial. Web what is the process for obtaining a prior authorization? Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. Web prior authorization, step therapy, & quantity limitations; You may opt out of future communications at any time. Web the portal is the preferred method for the submission of prior authorization requests, however requests can still be sent via fax by completing the new prior. Web our plan has a team of doctors and pharmacists who create tools to help us provide you quality coverage. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web pharmacy forms & notices. Web prior authorization, enter therapy, & package limit;
Covermymeds Humana Prior Auth Form Medco Prior Authorization Form
Web pharmacy forms & notices. Web however, a completed written authorization is required prior to processing a request. We require you to get. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. If you have questions about.
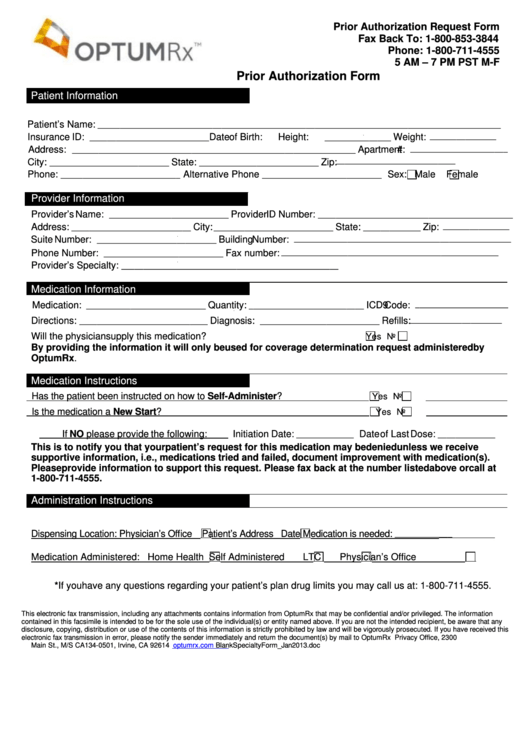
Aarp Optumrx Prior Authorization Form Form Resume Examples EVKYM0oK06
Web prior authorization, enter therapy, & package limit; Protect yourself against medicare fraud and identifies. Web ascension complete will continue to perform prior authorization of coverage for interventional imaging procedures (even those that utilize mr/ct technology) prior. Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. * to process request, all.
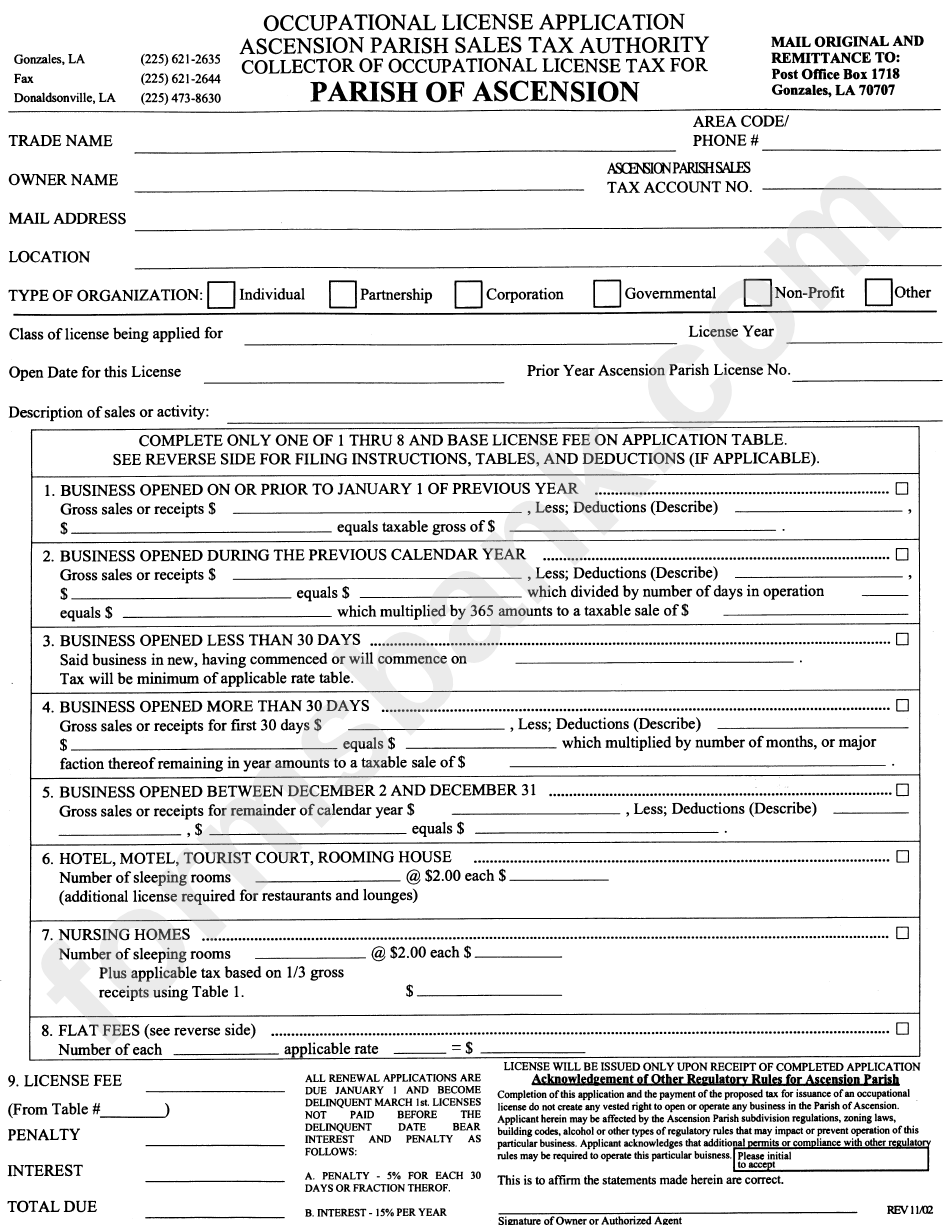
Occupational License Application Form Parish Of Ascension printable
Web this documentation includes the following: Web however, a completed written authorization is required prior to processing a request. Web prior authorization, step therapy, & quantity limitations; You may begin the steps for a prior authorization by contacting member services. Web city * state * zip/postal code * by completing this form, you give ascension complete permission to contact you.
Aarp Medicare Rx Prior Auth Form Universal Network
Web the portal is the preferred method for the submission of prior authorization requests, however requests can still be sent via fax by completing the new prior. We require you to get. Web clinicians can submit requests: If you have questions about. The um provider portal is an all access entry into your prior authorization requests and determinations.
Aarp Medicare Part B Prior Authorization Form Form Resume Examples
Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. If you have questions about. By portal view the status of an authorization by visiting the clinician portal by fax fax a completed prior authorization form to: Web however, a completed written authorization is required prior to processing a request. • diagnostic.
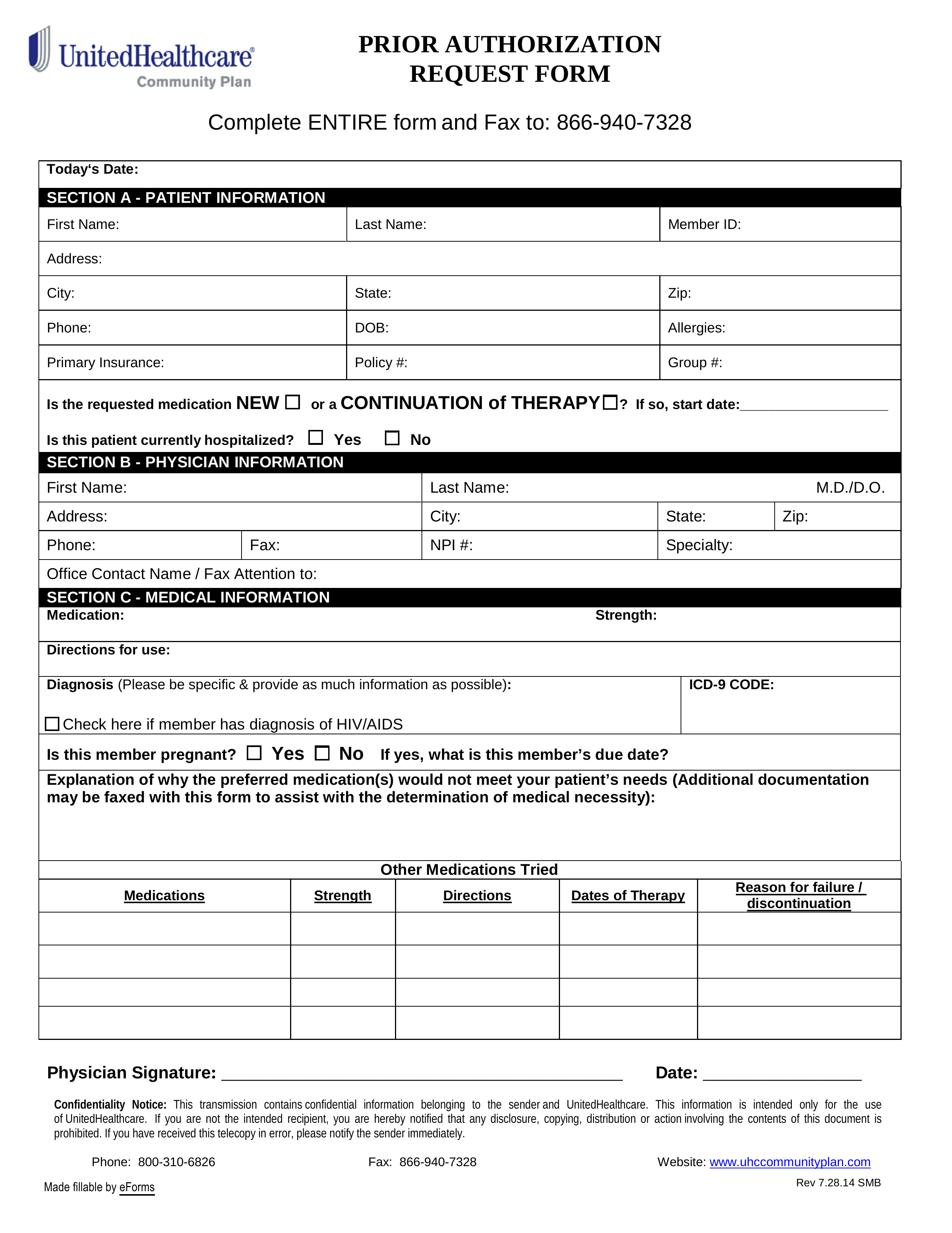
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
Web what is the process for obtaining a prior authorization? * to process request, all required fields with asterisks. Web prior authorization, step therapy, & quantity limitations; Web provider resources | ascension complete | 2020 prior authorization forms medicare parts: You may opt out of future communications at any time.
Healthsmart Prior Authorization Request Form Fill Online, Printable
• smarthealth prior authorization form filled out in its entirety • clinical notes outlining symptoms and their duration • physical exam. Web this documentation includes the following: Web prior authorization, enter therapy, & package limit; Web just go to the information center and click on a section labeled “prior authorization.” the next step is completing the prior authorization form. Web.
Ascension Parish Sales And Use Tax Authority Fill Online, Printable
Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. You may opt out of future communications at any time. By portal view the status of an authorization by visiting the clinician portal by fax fax a completed prior authorization form to: Web prior authorization, step therapy, & quantity limitations; Protect yourself.
Fillable Prior Authorization Request Form printable pdf download
We require you to get. You may begin the steps for a prior authorization by contacting member services. Web prior authorization, enter therapy, & package limit; Web our plan has a team of doctors and pharmacists who create tools to help us provide you quality coverage. If you have questions about.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Web object moved to here. Web our plan has a team of doctors and pharmacists who create tools to help us provide you quality coverage. You may opt out of future communications at any time. Web what is the process for obtaining a prior authorization? The um provider portal is an all access entry into your prior authorization requests and.
• Diagnostic Imaging (Mr, Ct/Cta, Ccta, Pet, Myocardial.
Web pharmacy forms & notices. Web just go to the information center and click on a section labeled “prior authorization.” the next step is completing the prior authorization form. By portal view the status of an authorization by visiting the clinician portal by fax fax a completed prior authorization form to: Web what is the process for obtaining a prior authorization?
Web Prior Authorization, Enter Therapy, & Package Limit;
Web clinicians can submit requests: We require you to get. Web ascension complete will continue to perform prior authorization of coverage for interventional imaging procedures (even those that utilize mr/ct technology) prior. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage.
Web The Portal Is The Preferred Method For The Submission Of Prior Authorization Requests, However Requests Can Still Be Sent Via Fax By Completing The New Prior.
* to process request, all required fields with asterisks. Web our plan has a team of doctors and pharmacists who create tools to help us provide you quality coverage. If you have questions about. Web prior authorization, step therapy, & quantity limitations;
The Um Provider Portal Is An All Access Entry Into Your Prior Authorization Requests And Determinations.
You may begin the steps for a prior authorization by contacting member services. You may opt out of future communications at any time. • smarthealth prior authorization form filled out in its entirety • clinical notes outlining symptoms and their duration • physical exam. Web object moved to here.