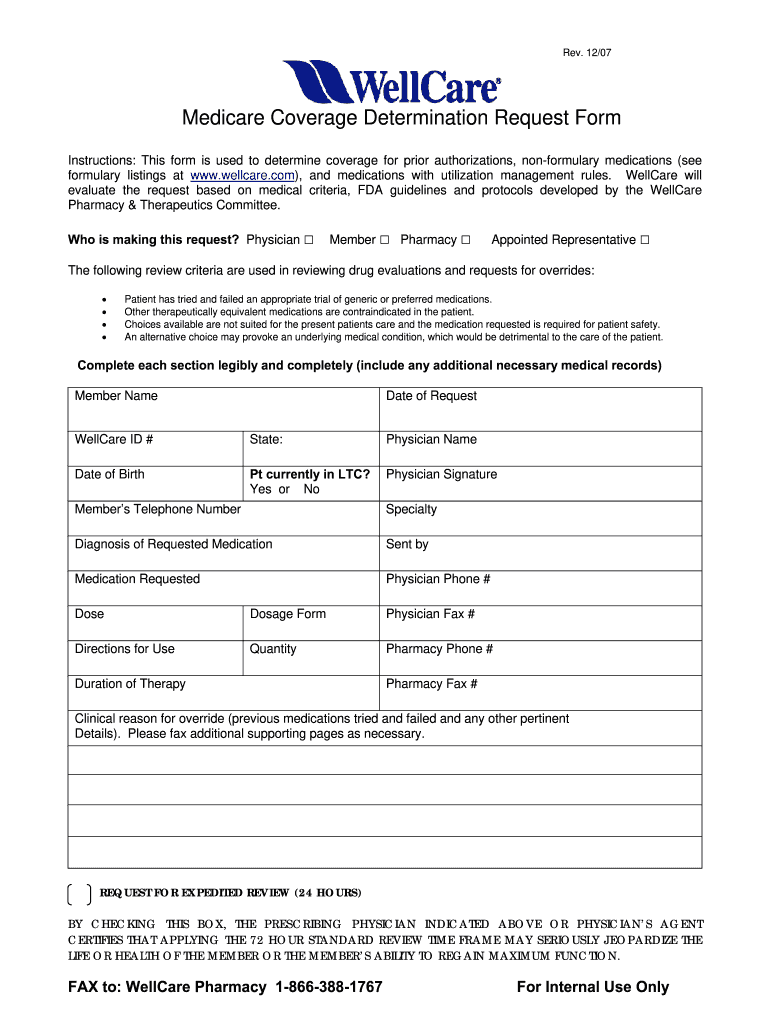
Allwell Prior Auth Form
Allwell Prior Auth Form - Copies of all supporting clinical information are required. Copies of all supporting clinical information are required. This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by allwell. Web prior authorizations for musculoskeletal procedures should be verified by turningpoint. Complex imaging, mra, mri, pet and ct scans need to be verified by nia. Prior authorization, step therapy, & quantity limitations; Web what is the process for obtaining a prior authorization? Determination made as expeditiously as the enrollee’s health condition requires, but no later than 14 calendar days after receipt of request. Web allwell pharmacy updates effective may 1, 2019; Meridian street, suite 101 indianapolis, in 46204.
Web allwell prior authorization changes effective august 1, 2021 (pdf) point of care formulary information (pdf) updated: Determination made as expeditiously as the enrollee’s health condition requires, but no later than 14 calendar days after receipt of request. Web authorization form all required fields must be filled in as incomplete forms will be rejected. Don’t risk losing your kancare benefits. All required fields must be filled in as incomplete forms will be rejected. Don’t risk losing your kancare benefits. Web pharmacy policies & forms coverage determinations and redeterminations. This notice contains information regarding such prior authorization requirements and is applicable to all medicare products offered by allwell. Copies of all supporting clinical information are required. Lack of clinical information may result in delayed determination.
Lack of clinical information may result in delayed determination. All required fields must be filled in as incomplete forms will be rejected. Musculoskeletal services need to be verified by turningpoint. Web pharmacy policies & forms coverage determinations and redeterminations. Web prior authorization, step therapy, & quantity limitations; Home find a doctor careers login contact contrast a a a kancare: Prior authorization should be requested at least five (5) days before the scheduled service delivery date or as soon as need for service is identified. We recommend that providers submit prior authorizations through the web portal, via phone or via fax. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Complex imaging, mra, mri, pet and ct scans need to be verified by nia.
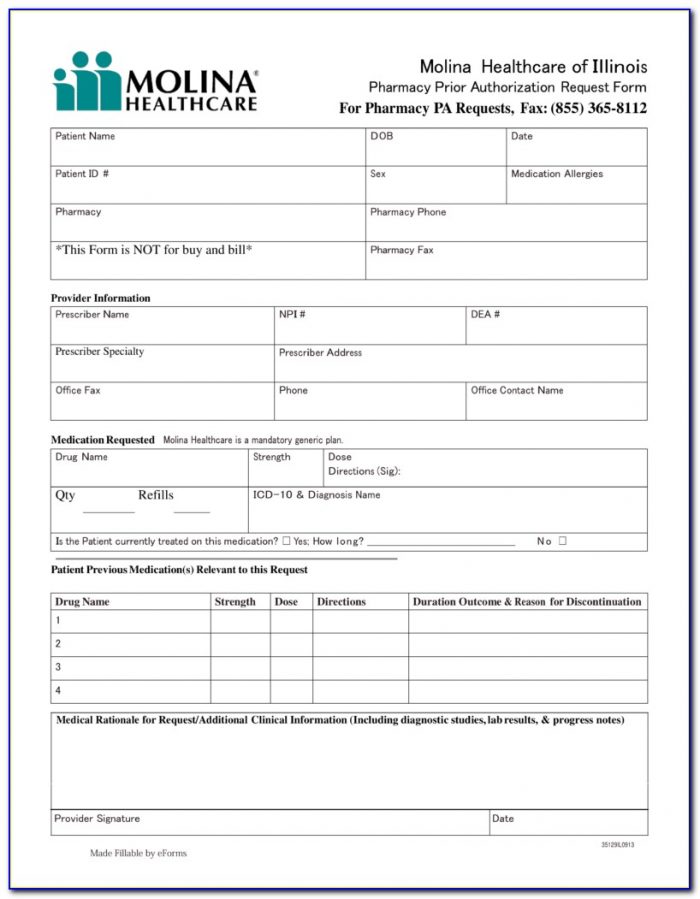
Medicare Advantage Medication Prior Authorization Forms Form Resume
Prior authorization should be requested at least five (5) days before the scheduled service delivery date or as soon as need for service is identified. Lack of clinical information may result in delayed determination. Web what is the process for obtaining a prior authorization? Lack of clinical information may result in delayed determination. Complex imaging, mra, mri, pet and ct.
Prior Auth Form For Medicare Part D Universal Network
Lack of clinical information may result in delayed determination. Lack of clinical information may result in delayed determination. Web pharmacy policies & forms coverage determinations and redeterminations. Prior authorization, step therapy, & quantity limitations. Copies of all supporting clinical information are required.
Standard Pharmacy Prior Authorization Form for Prepaid Health Plans
Prior authorization, step therapy, & quantity limitations. Web authorization form all required fields must be filled in as incomplete forms will be rejected. We recommend that providers submit prior authorizations through the web portal, via phone or via fax. Web as a reminder, all planned/elective admissions to the inpatient setting require prior authorization. Access key forms for authorizations, claims, pharmacy.
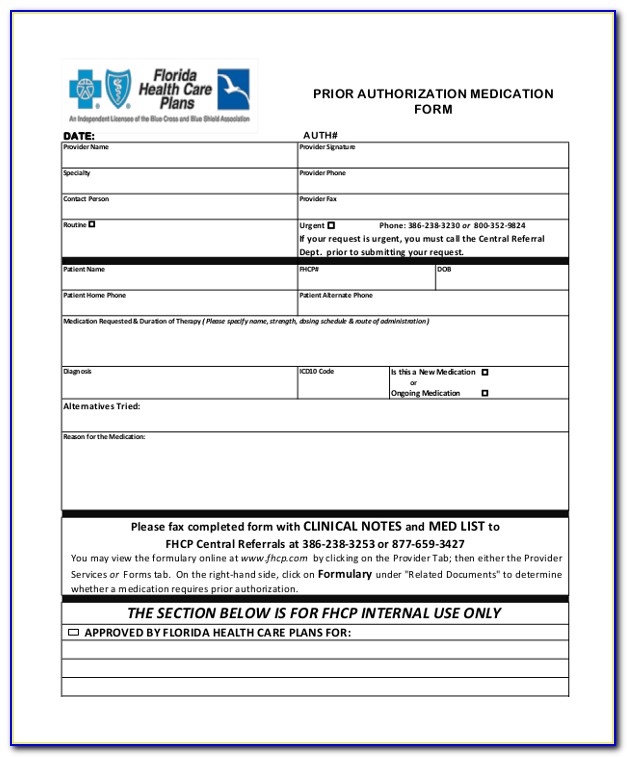
Wellcare Forms For Prior Authorization Fill Out and Sign Printable
Web allwell from home state health prior authorization updates allwell from home state health requires prior authorization as a condition of payment for many. Web allwell prior authorization changes effective august 1, 2021 (pdf) point of care formulary information (pdf) updated: Web pharmacy policies & forms coverage determinations and redeterminations. All required fields must be filled in as incomplete forms.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
We recommend that providers submit prior authorizations through the web portal, via phone or via fax. Prior authorization, step therapy, & quantity limitations; Lack of clinical information may result in delayed determination. Copies of all supporting clinical information are required. Web prior authorization, step therapy, & quantity limitations;
Wellcare Medicare Medication Prior Authorization Form Form Resume
The outpatient prior authorization form can be found on our website at superior’s provider forms webpage. Web allwell prior authorization changes effective august 1, 2021 (pdf) point of care formulary information (pdf) updated: Web allwell pharmacy updates effective may 1, 2019; Web allwell from buckeye health plan requires prior authorization as a condition of payment for many services. Determination made.
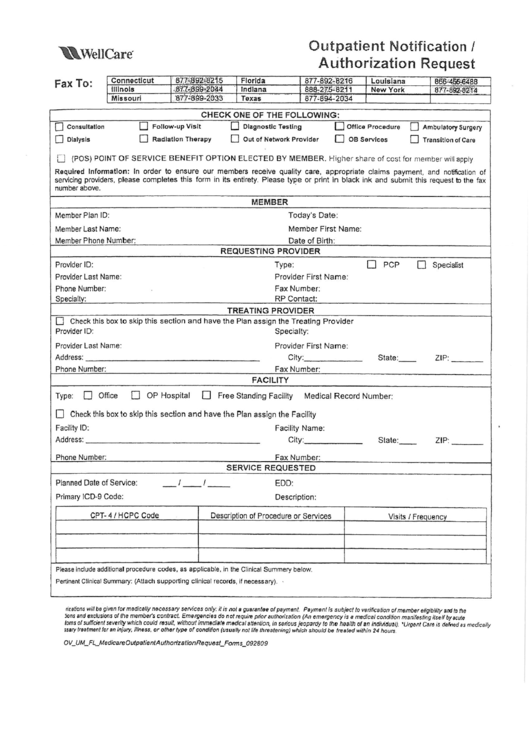
Fillable Outpatient Notification /authorization Request Wellcare
All required fields must be filled in as incomplete forms will be rejected. Lack of clinical information may result in delayed determination. Prior authorization, step therapy, & quantity limitations; Web authorization form all required fields must be filled in as incomplete forms will be rejected. Medicare inpatient prior authorization fax form (pdf) medicare outpatient prior authorization fax form (pdf) medicare.
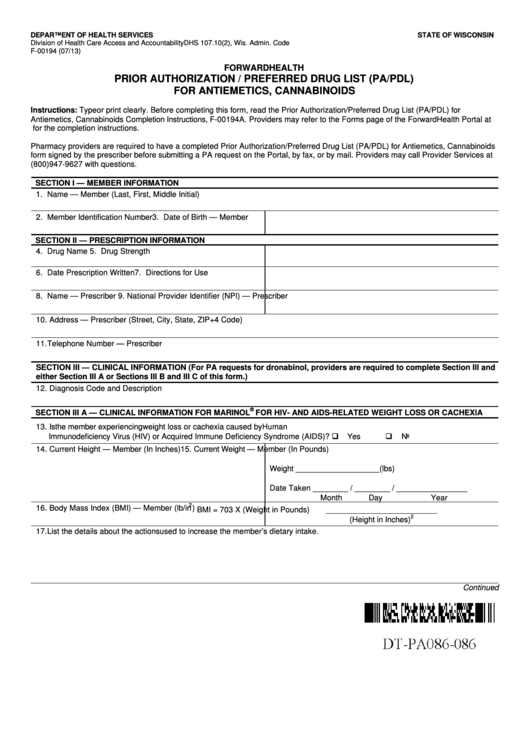
Prior Authorization / Preferred Drug List printable pdf download
Access key forms for authorizations, claims, pharmacy and more. Determination made as expeditiously as the enrollee’s health condition requires, but no later than 14 calendar days after receipt of request. Web prior authorizations for musculoskeletal procedures should be verified by turningpoint. Web allwell from home state health prior authorization updates allwell from home state health requires prior authorization as a.
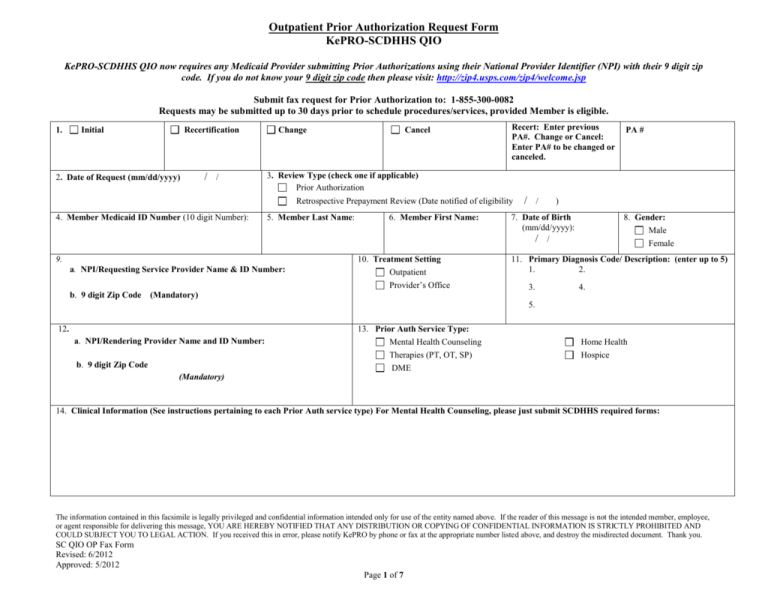
Outpatient Prior Authorization Request Fax Form
Copies of all supporting clinical information are required. Lack of clinical information may result in delayed determination. Determination made as expeditiously as the enrollee’s health condition requires, but no later than 14 calendar days after receipt of request. Prior authorization, step therapy, & quantity limitations; Web as a reminder, all planned/elective admissions to the inpatient setting require prior authorization.
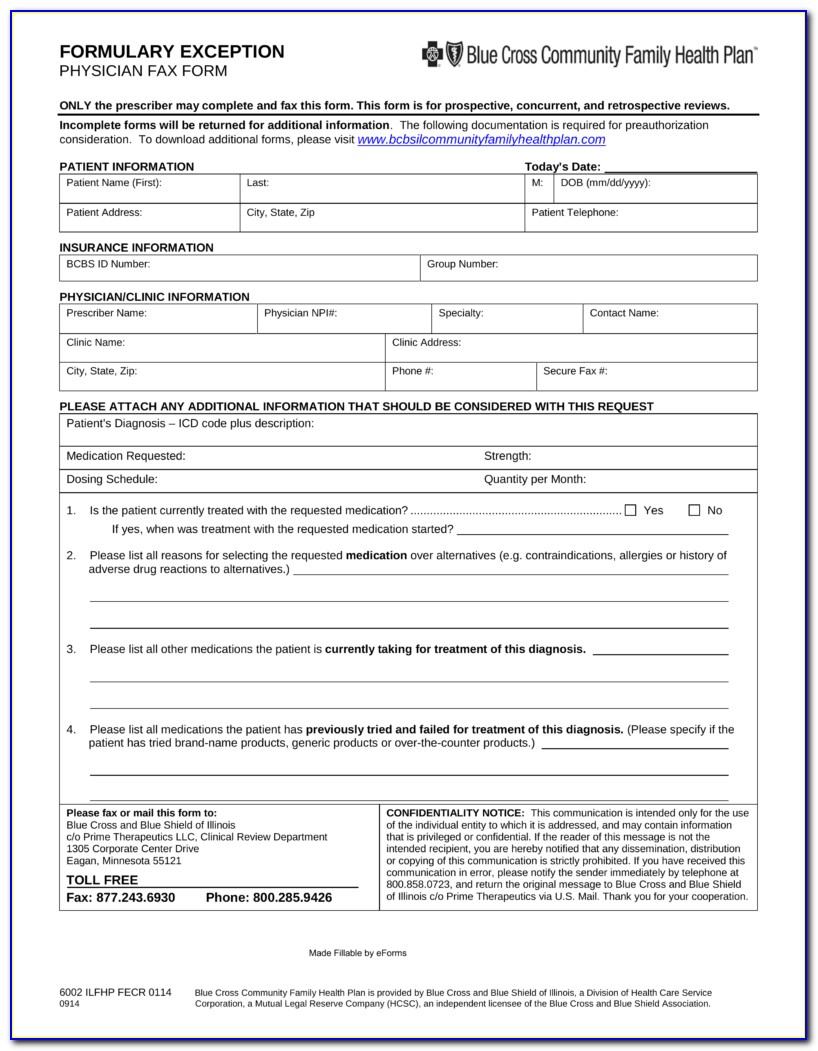
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
The fax authorization form can be found. Prior authorization is a process initiated by the. Complex imaging, mra, mri, pet and ct scans need to be verified by nia. Web pharmacy policies & forms coverage determinations and redeterminations. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response.
Prior Authorization Should Be Requested At Least Five (5) Days Before The Scheduled Service Delivery Date Or As Soon As Need For Service Is Identified.
Web what is the process for obtaining a prior authorization? Wellcare by allwell 550 n. You may request prior authorization by contacting member services. The outpatient prior authorization form can be found on our website at superior’s provider forms webpage.
Web Allwell Pharmacy Updates Effective May 1, 2019;
Access key forms for authorizations, claims, pharmacy and more. Meridian street, suite 101 indianapolis, in 46204. Copies of all supporting clinical information are required. Medicare inpatient prior authorization fax form (pdf) medicare outpatient prior authorization fax form (pdf) medicare provider reference card.
Prior Authorization, Step Therapy, & Quantity Limitations.
Web allwell from home state health prior authorization updates allwell from home state health requires prior authorization as a condition of payment for many. Web authorization form all required fields must be filled in as incomplete forms will be rejected. Home find a doctor careers login contact contrast a a a kancare: Web as a reminder, all planned/elective admissions to the inpatient setting require prior authorization.
Lack Of Clinical Information May Result In Delayed Determination.
Complex imaging, mra, mri, pet and ct scans need to be verified by nia. All required fields must be filled in as incomplete forms will be rejected. Web allwell from buckeye health plan requires prior authorization as a condition of payment for many services. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor.